1 Friedman DS, O’Colmain BJ, Munoz B, Tomany SC, McCarty C, De Jong PT, Nemesure B, Mitchell P, Kempen J. Prevalence of age-related macular degeneration in the United States. Arch ophthalmic. 2004 Apr 1;122(4):564-72.
2 Sobrin L, Seddon JM. Nature and nurture-genes and environment-predict onset and progression of macular degeneration. Progress in retinal and eye research. 2014 May 1; 40:1-5.
3 Rosenfield PJ, Martidis A, Tennant M. Age-related macular degeneration. In: Yanoff M, Duker JS, Augsburger JJ, eds. Ophthalmology: Expert Consult. 3rd ed. Philadelphia, PA: Elsevier Mosby; 2009.
4 Shalev V, Sror M, Goldshtein I, Kokia E, Chodick G. Statin use and the risk of age-related macular degeneration in a large health organization in Israel. Ophthalmic epidemiology. 2011 Apr 1;18(2):83-90.
5 Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, Wong TY. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. The Lancet Global Health. 2014 Feb 1;2(2): e106-16.
6 Cheung LK, Eaton A. Age‐related macular degeneration. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy. 2013 Aug;33(8):838-55.
7 Delcourt C, Souied E, Sanchez A, Bandello F. Development and validation of a risk score for age-related macular degeneration: the STARS Questionnaire. Investigative Ophthalmology & Visual Science. 2017 Dec 1;58(14):6399-407.
8 Bucan K, Lukic M, Bosnar D, Kopic A, Jukic T, Konjevoda S, Glavadanovic S, Gverovic Antunica A. Analysis of association of risk factors for age-related macular degeneration. European Journal of Ophthalmology. 2022 Jan;32(1):410-6.
9 Fong DS. Age-related macular degeneration: update for primary care. American Family Physician. 2000 May 15;61(10):3035-42.
10 Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, Kamei M, Hasan A, Yan L, Rayborn ME, Salomon RG. Drusen proteome analysis: an approach to the aetiology of age-related macular degeneration. Proceedings of the National Academy of Sciences. 2002 Nov 12;99(23):14682-7.
11 Bressler NM, Bressler SB, West SK, Fine SL, Taylor HR. The grading and prevalence of macular degeneration in Chesapeake Bay watermen. Archives of Ophthalmology. 1989 Jun 1;107(6):847-52.
12 Sarks JP, Sarks SH, Killingsworth MC. Evolution of soft drusen in age-related macular degeneration. Eye. 1994 May;8(3):269-83.
13 Klein R, Davis MD, Magli YL, Segal P, Klein BE, Hubbard L. The Wisconsin age-related maculopathy grading system. Ophthalmology. 1991 Jul 1;98(7):1128-34.
14 Ferris FL, Davis MD, Clemons TE, Lee LY, Chew EY, Lindblad AS, Milton RC, Bressler SB, Klein R. A simplified severity scale for age-related macular degeneration: AREDS Report No. 18. Archives of ophthalmology (Chicago, Ill.: 1960). 2005 Nov 1;123(11):1570-4.
15 Klein ML, Francis PJ, Ferris FL, Hamon SC, Clemons TE. Risk assessment model for development of advanced age-related macular degeneration. Archives of ophthalmology. 2011 Dec 1;129(12):1543-50.
16 Klein ML, Ferris III FL, Armstrong J, Hwang TS, Chew EY, Bressler SB, Chandra SR, AREDS Research Group. Retinal precursors and the development of geographic atrophy in age-related macular degeneration. Ophthalmology. 2008 Jun 1;115(6):1026-31.
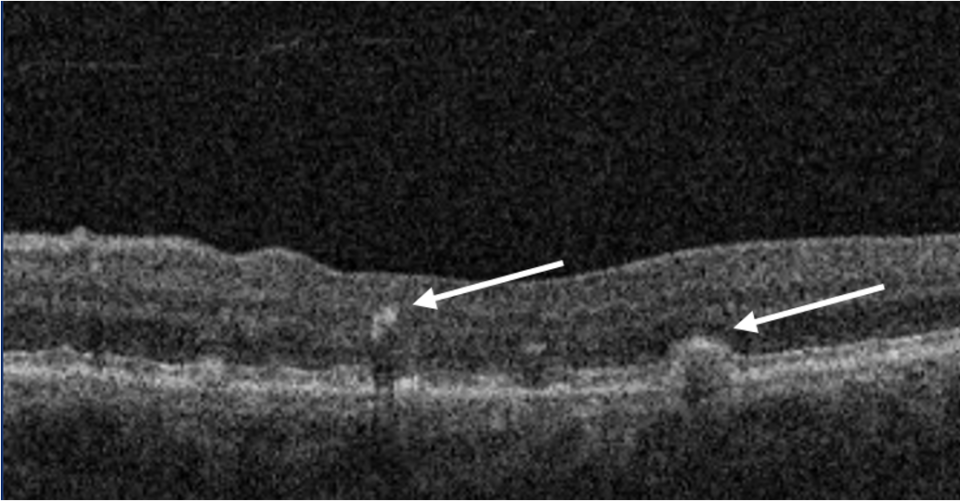
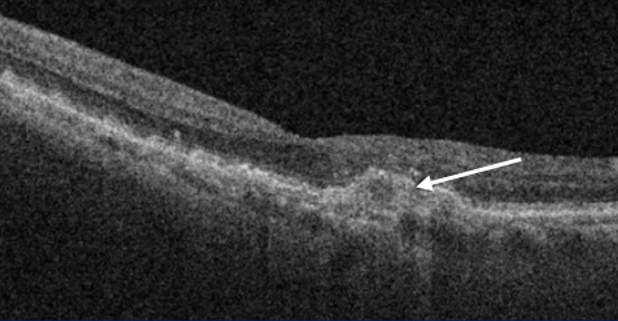
17 Chen L, Messinger JD, Zhang Y, Spaide RF, Freund KB, Curcio CA. Subretinal drusenoid deposit in age-related macular degeneration: histologic insights into initiation, progression to atrophy, and imaging. Retina (Philadelphia, Pa.). 2020 Apr;40(4):618.
18 Spaide RF, Ooto S, Curcio CA. Subretinal drusenoid deposits AKA pseudodrusen. Survey of ophthalmology. 2018 Nov 1;63(6):782-815.
19 Fleckenstein M, Mitchell P, Freund KB, Sadda S, Holz FG, Brittain C, Henry EC, Ferrara D. The progression of geographic atrophy secondary to age-related macular degeneration. Ophthalmology. 2018 Mar 1;125(3):369-90.
20 Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Archives of ophthalmology. 2001 Oct 1;119(10):1417-36.
21 Chew EY, Clemons TE, SanGiovanni JP, Danis R, Ferris FL, Elman M, Antoszyk A, Ruby A, Orth D, Bressler S, Fish G. Lutein+ zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA-Journal of the American Medical Association. 2013 May 15;309(19):2005-15.
22 Gopinath B, Liew G, Kifley A, Lewis JR, Bondonno C, Joachim N, Hodgson JM, Mitchell P. Association of dietary nitrate intake with the 15-year incidence of age-related macular degeneration. Journal of the Academy of Nutrition and Dietetics. 2018 Dec 1;118(12):2311-4.
23 Neelam K, Zhou SW, Eong KG. The role of blue light in the pathogenesis of age-related macular degeneration. Points de Vue. 2014(71):77.
24 https://investors.apellis.com/news-releases/news-release-details/apellis-completes-enrollment-two-phase-3-studies-targeted-c3
25 Jaffe GJ, Westby K, Csaky KG, Monés J, Pearlman JA, Patel SS, Joondeph BC, Randolph J, Masonson H, Rezaei KA. C5 inhibitor avacincaptad pegol for geographic atrophy due to age-related macular degeneration: a randomized pivotal phase 2/3 trial. Ophthalmology. 2021 Apr 1;128(4):576-86.
26 Liao DS, Grossi FV, El Mehdi D, Gerber MR, Brown DM, Heier JS, Wykoff CC, Singerman LJ, Abraham P, Grassmann F, Nuernberg P. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology. 2020 Feb 1;127(2):186-95.