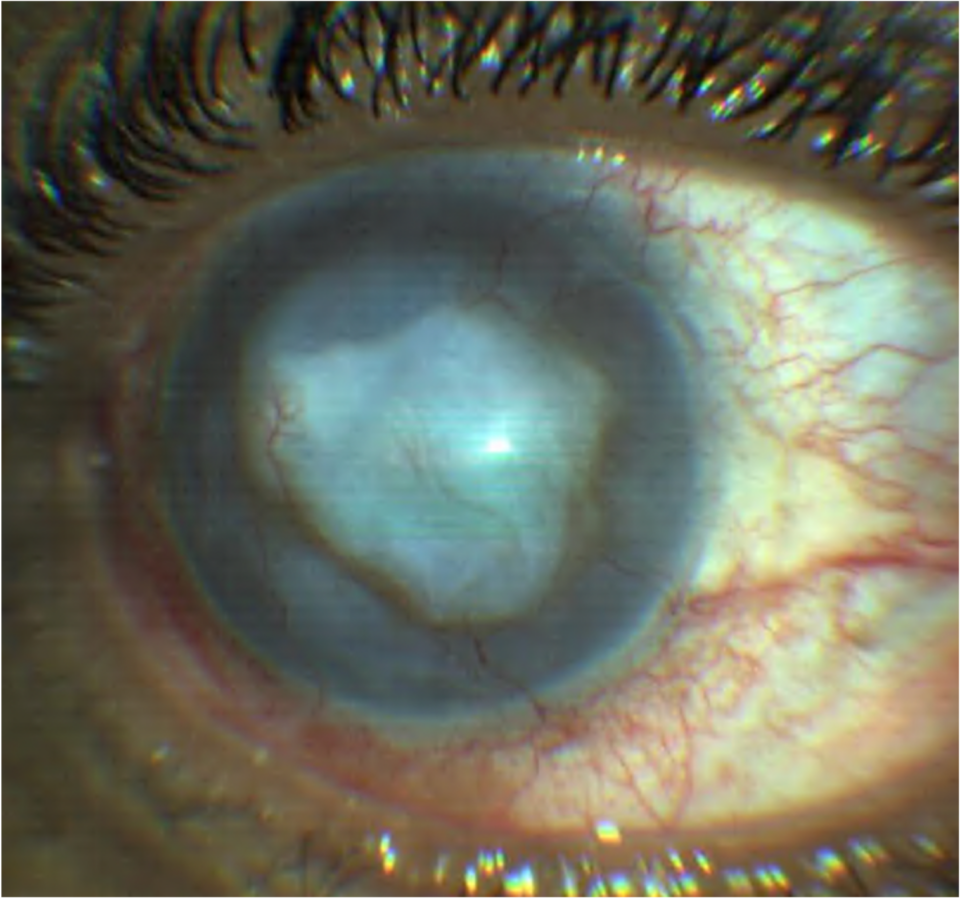
Bullous keratopathy refers to irreversible corneal oedema secondary to damage to the corneal endothelium. The most common cause is cataract surgery and intraocular (IOL) lens implantation; therefore, in literature is known as pseudophakic bullous keratopathy.(1,2) The bullous keratopathy may occur in aphakic eyes or in Fuchs’s corneal dystrophy.(3)
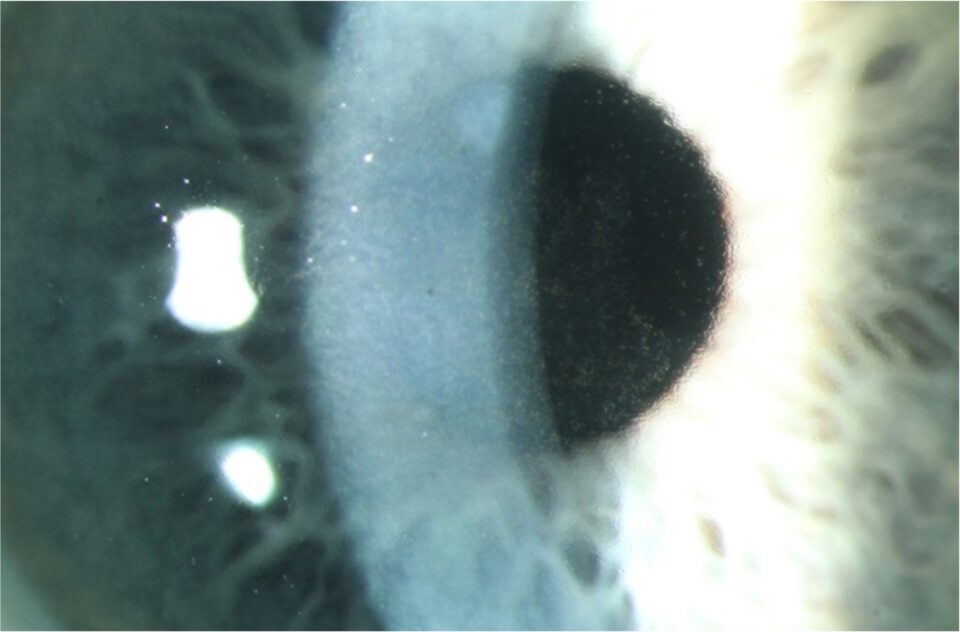
The cornea, to be transparent, needs to maintain a dehydrated state. The corneal endothelium is significant in keeping the cornea transparent, where endothelial cells work as a pump.(4) Any damage to the corneal endothelium brings a risk of developing corneal oedema and, consequently, bullous keratopathy. Firstly, the fluid enters the cornea’s stroma and then the epithelium. Epithelial oedema manifests with bullae. Therefore, bullous keratopathy refers to the condition’s name. The endothelial cell density has decreased since birth, and the typical average cell density in an adult person is 2500-2700 cells/mm2. There must be a critically decreased cell density for bullous keratopathy to develop. The published studies revealed that bullous keratopathy occurs when the cell density is lower than 700 cells/mm2 or 300-500 cells/mm2.(1,5) It’s been thought that post, intra-, and post-operative cell loss contribute to the development of bullous keratopathy.(1)
Risk factors cause lower pre-operative endothelial cell density, like advanced age, pre-existing corneal Fuchs’s dystrophy, shallow anterior chamber, glaucoma, previous ocular trauma, diabetes, and chronic obstructive pulmonary disease.(6,7( Fuchs dystrophy is a genetic disorder that causes bilateral, progressive corneal endothelial cell loss, sometimes leading to symptomatic bullous keratopathy by age 50 to 60.(3)
It is estimated that 1-2% of people will develop persistent post-operative corneal oedema. Improving surgical techniques and the design of intraocular lenses improved the incidence of bullous keratopathy. Surgical trauma and pre-operative endothelial cell density are the main risk factors for developing the condition.(2)