Hypertension is the leading risk factor for cardiovascular disease (CVD) and mortality worldwide, with a projected number of 1.56 billion individuals with hypertension by 2025.(1,2)
The American College of Cardiology/American Heart Association (ACC/AHA) suggested the following definitions for high blood pressure in 2017.(3)
| Category |
Systolic (SBP) |
Diastolic (DBP) |
| Elevated blood pressure |
120-129 mmHg |
< 80 mmHg |
| Stage 1 hypertension |
130-139 mmHg |
80-89 mmHg |
| Stage 2 hypertension |
≥ 140 mmHg |
≥ 90 mmHg |
Hypertension profoundly affects the vasculature’s structure and function in the eye. This results in various clinical signs representing hypertensive retinopathy, choroidopathy, and optic neuropathy. Hypertensive retinopathy is the most common clinical presentation. In addition, hypertension may cause occlusion of the main retinal vessels, representing retinal artery or retinal vein occlusions (both branch and central).
Hypertensive retinopathy ranges from 2-17% in non-diabetic patients, but the prevalence varies by demographic group.(4) Hypertensive retinopathy is more common among African, American, and Chinese individuals. Risk factors for essential hypertension include a high salt diet, obesity, tobacco use, alcohol, family history, stress, and ethnic background. -The duration of high blood pressure is the primary risk factor for arteriosclerotic hypertensive retinopathy. In contrast, the degree of blood pressure elevation beyond normal levels is the major risk factor for malignant hypertension.(5)
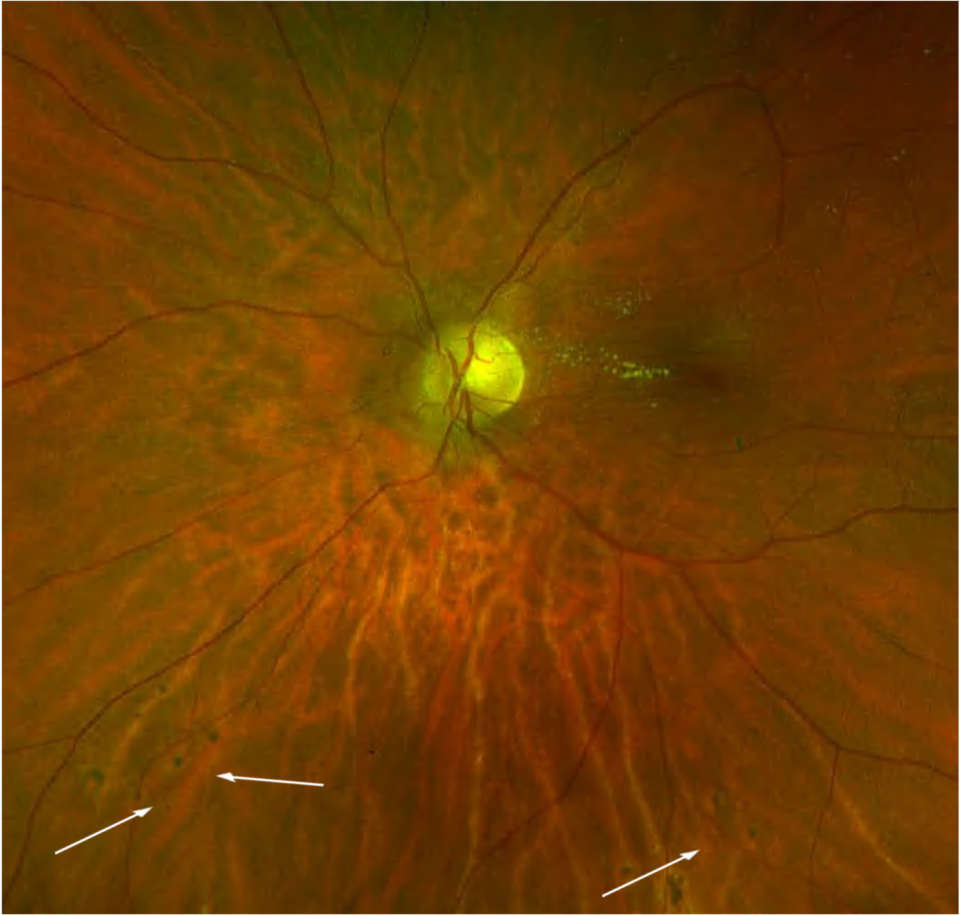
The initial phase of hypertensive retinopathy is called the vasoconstrictive phase. High blood pressure affects the vascular muscles tonus, which consequently causes constriction of the arterioles (controls the retinal blood flow). Clinically, it represents arteriolar narrowing (focal or generalised). Some studies suggest that arterial narrowing may be a preclinical marker of hypertension, as some patients may not have developed clinical hypertension yet.(6) Persistently elevated blood pressure leads to the sclerotic phase, which causes thickening of the intima of blood vessels and media wall hyperplasia (structural changes of retinal arterioles). This stage accords with diffused and localised (focal) retinal arteriolar narrowing, arteriolar wall opacification (“silver” or “copper wiring”), and compression of the venules by structural changes in the arterioles (arteriovenous “nicking” or “nipping”). Furthermore, chronically elevated blood pressure disrupts the blood-retinal barrier, which is secondary to necrosis of both smooth muscles of retinal vessels and endothelial cells. -. Retinal microaneurysms, haemorrhages, lipid exudates, and cotton wool spots characterise the exudative phase. (7) Very high blood pressure, which occurs rapidly (above 180/120 mmHg), causes signs of malignant hypertensive retinopathy. Clinically, it manifests with signs of the exudative phase, including optic disc swelling and lipid exudates in the macula.
Recent research findings suggest that generalised retinal arteriolar narrowing and arteriovenous nicking are not only associated with current blood pressure levels but also with blood pressure levels measured in the past. These findings suggest that these retinal signs reflect the cumulative effects of longstanding hypertension and serve as persistent markers of chronic hypertensive damage. On the other hand, focal arteriolar narrowing, retinal haemorrhages, microaneurysms, and cotton-wool spots are associated explicitly with concurrently measured blood pressure levels. These retinal signs mirror the effects of short-term blood pressure changes rather than reflecting the cumulative impact of longstanding hypertension. (8)
In addition, studies found that retinal venular widening or dilation is also related to high blood pressure levels and incident hypertension.
Based on the above description of different stages of the disease, hypertensive retinopathy can be classified as follows(11):
- No signs of hypertensive retinopathy
- Mild: Generalised arteriolar narrowing, focal arteriolar narrowing, arteriovenous nicking, arteriolar wall opacification (silver or copper wiring), or a combination of these signs.
- Moderate: Haemorrhages (blot, dot, or flame-shaped), microaneurysms, cotton-wool spots, hard exudates, or a combination of these signs.
- Malignant: Signs of moderate retinopathy in combination with optic disc swelling in the presence of severely elevated blood pressure.