Material and design matter
Scientists and practitioners have questioned the influence of polymer chemistry, and various other material attributes that can be measured and quantified. The considered attributes are:
- The bulk, such as water content, dehydration, Ionicity, oxygen transmissibility, modulus and mechanical factors.
- The surface properties, such as friction, wettability, surface modification of contact lens materials.
- Contact lens material chemistry.
Up to now, almost none of these attributes – with the possible exception of friction – appears to be associated directly with contact lens discomfort. Contact lenses of different brands and manufacturers will vary in terms of their design. As a practitioner, you probably recognise that the design of contact lenses affects their ability to fit the ocular surface properly and that this influences the overall performance. For example, for soft contact lenses, moderate on-eye movement (with tear exchange) and corneal coverage are essential, but its overall association with contact lens discomfort is not entirely clear. There is even less consensus about the influence of various design attributes on the condition. However, friction, size, shape, and contour of lens edges appear to be some of the most influential determinants of contact lens comfort for soft contact lenses.
Better care, better comfort
Contact lens care solutions, practices, and wear schedules are interesting when we look at understanding their role(s) in contact lens discomfort. Peer-reviewed literature doesn’t show specific formulations or components that may be associated with either increasing the discomfort or improving comfort. That said, we can probably all agree that regular contact lens care – including rub, rinse, and adequate soaking – is essential in wearing contact lenses comfortably. Also, replacing soft contact lenses regularly is best for ocular health, and could potentially improve comfort.
What about patient- and environment-related factors?
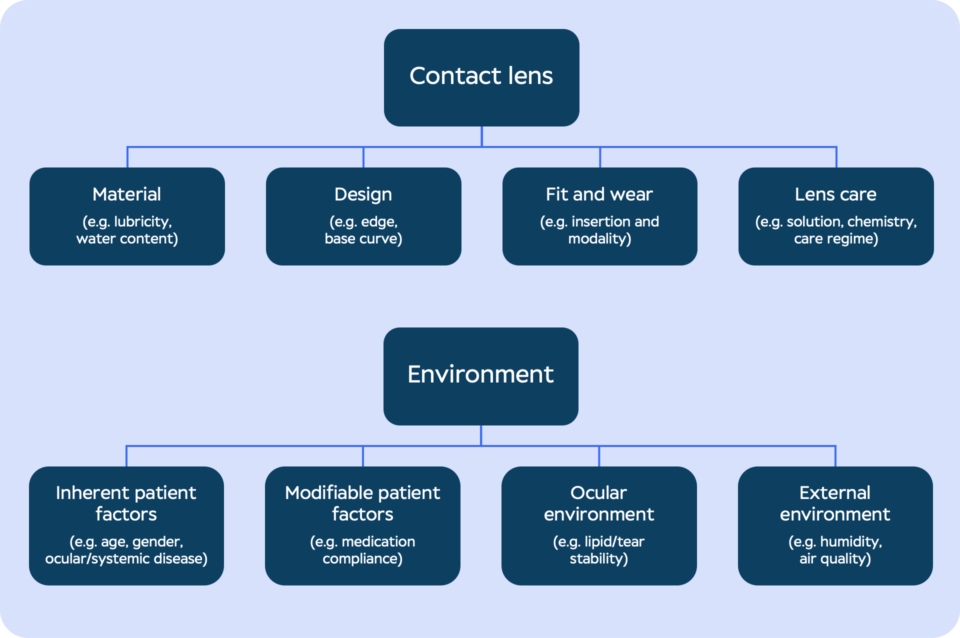
Apart from contact lens material, design, and care, the classification scheme in figure 1 also shows that there are several patient- and environment-related factors that can cause contact lens discomfort.
It shouldn’t be a surprise that the eye can detect and sometimes react to the presence of a contact lens – as the contact lens touches sensitive parts, like the cornea, lid margin and, to a lesser extent, the conjunctiva. Evidence from the literature shows some occasional patient-related factors associated with the condition, such as female sex, younger age, inadequate tear film quantity and quality, seasonal allergies, and the use of systemic medications. On the other hand, there is little evidence that ethnicity, blink rate and blinking patterns, systemic disease, diet, alcohol, smoking, cosmetic use, or psychological factors play a role in contact lens discomfort.
The TFOS report also indicates that literature supports that symptoms of contact lens discomfort can occur due to an increased tear evaporation rate from the lens surface, because of a reduction in the relative humidity. In addition to this, the movement of air (wind) and visual activities that make people blink less (such as the use of digital devices) may worsen signs and symptoms of the condition. For the role of other environmental factors on contact lens discomfort, such as temperature, altitude, smoky environments, air conditioning or indoor heating, there’s little concrete evidence.