A symptomatic retinal artery occlusion is an ophthalmic emergency that requires immediate evaluation and transfer to a stroke centre.
The estimated incidence of central retinal artery occlusion (CRAO) is reported to be roughly 1 in 10,000 cases at specialised hospitals (tertiary referral centres), and even lower for the general population, at approximately 8.5 cases per 100,000.(1,2) The average age at presentation is in the early sixties, with more than 90% presenting at over 40 years. Men are affected more frequently.(3)
The ophthalmic artery is the main artery that supplies the eye and surrounding structures. The central retinal artery is the first branch of the ophthalmic artery, and it supplies nerve fibres in the optic nerve, as well as the inner layers of the retina. After entering the eye, the central retinal artery divides into superior and inferior branches. In addition, the cilioretinal artery is a branch of the short posterior ciliary arteries, a separate branch of the ophthalmic artery.(4)
The blockage may occur in any of the retinal artery or its branches, and may occur due to embolus, vasculitis, or spasm. In the literature, there are several entities described, based on the affected artery:
- Central retinal artery occlusion (CRAO)
- Branch retinal artery occlusion (BRAO)
- Cilioretinal retinal artery occlusion (CLRAO)
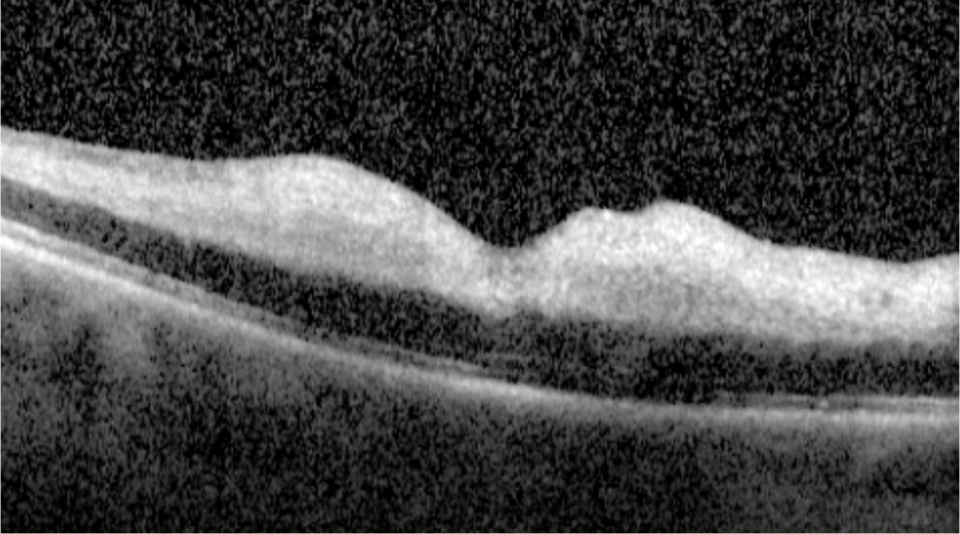
- Paracentral acute middle maculopathy (PAMM)
There are several risk factors for retinal artery occlusions: older age, male gender, smoking, hypertension, obesity, diabetes, hyperlipidaemia, cardiovascular disease, and coagulopathies.(5,6)
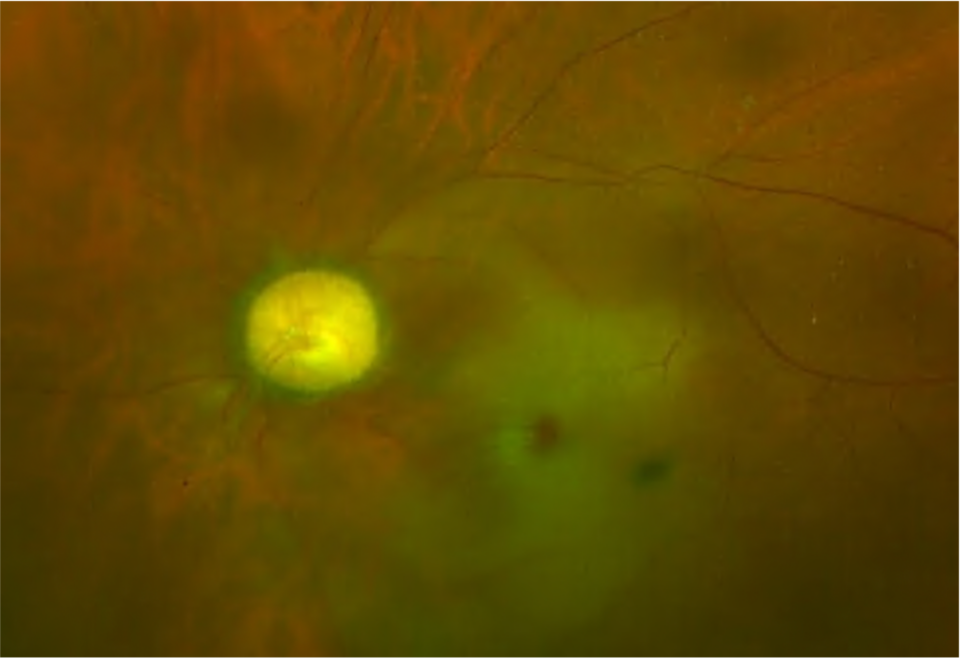
Retinal emboli are the most common cause of CRAO and BRAO.(7) The most common variant (74%) is a yellow, refractile cholesterol embolus (Hollenhorst plaque). They can also consist of calcified material (15.5%) or platelet and fibrin (15.5%).(8)
In central retinal artery occlusion, the inner retina is damaged. In branch retinal artery occlusions, representing 38% of all acute retinal artery occlusions, only part of the inner retinal perfusion is affected.(9) Cilioretinal artery occlusions account for 5% of all retinal artery occlusions and are often associated with central retinal vein occlusions.(10) Remember that 32% of the patients may have the presence of cilioretinal (according to angiography studies).(11) The PAMM is discovered in 2013 based on OCT findings, and it represents ischaemia of intermediate capillary plexus (ICP) and deep capillary plexus (DCP).(12)