- The ERM can contract and distort the retina leading to blurring and distortion of the vision.
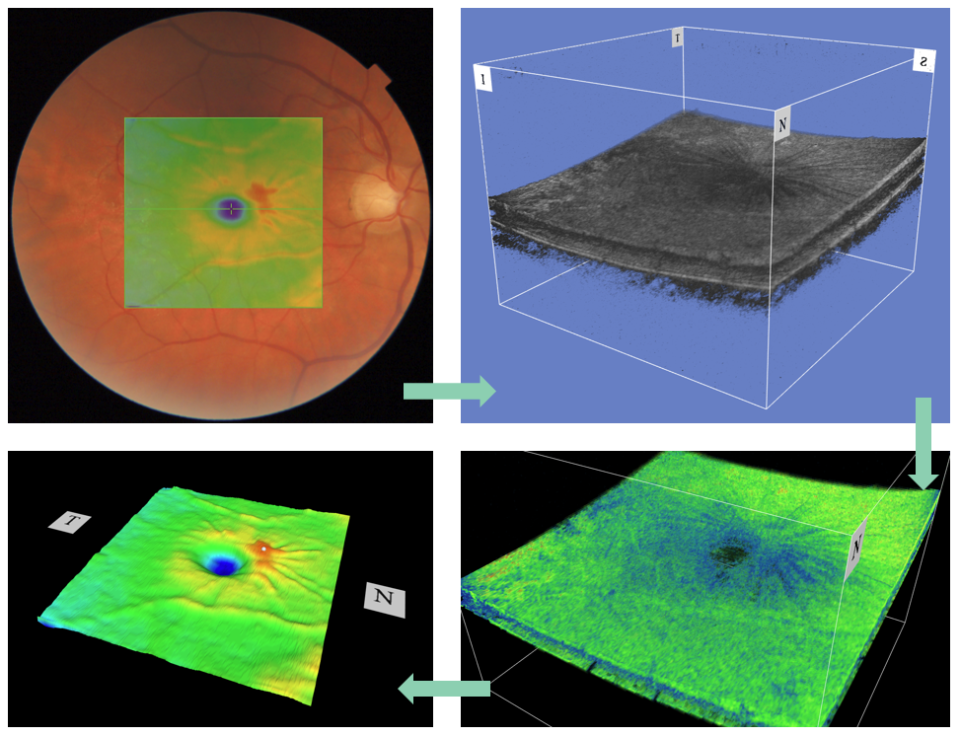
- ERMs can be very subtle and may not significantly affect vision for long periods of time. Other times they can progress more rapidly and cause bothersome visual symptoms. According to Gass, ERM can be classified into three categories:
- Grade 0 (cellophane maculopathy): a translucent membrane with no underlying retinal distortion.
- Grade 1 (wrinkled cellophane maculopathy): ERM with irregular wrinkling of the inner retina.
- Grade 2 (macula pucker): an opaque membrane causing obscuration of underlying vessels and marked full-thickness retinal distortion.

Sep 22, 2021
Chapter 4: Vitreomacular interface abnormalities
Introduction
The vitreomacular interface is a term for the vitreoretinal interface in the macular region. This chapter covers:
- Epiretinal membrane
- Vitreomacular traction
- Macular hole
Click on one of the cards below to read more about the specific eye condition.
Chapters
01
Epiretinal membrane
Referral: Normal if significant visual impact*
Occasionally a small film of tissue, like cellophane, grows on the centre of the retina (on the inner retinal surface). This condition is called an epiretinal membrane (ERM).
02
Vitreomacular traction
Referral: Normal if significant visual impact*
Vitreomacular traction (VMT) is a disorder of the vitreoretinal interface.
- With age, there is a sequential weakening of attachments between the vitreous and the internal limiting membrane of the retina, starting from the perifoveal region, superior and inferior vascular arcades, fovea, mid-peripheral retina and optic disc.
- Anteroposterior traction is caused by an incomplete posterior vitreous detachment, where the vitreous presents an abnormal strong adhesion to the macula.
- Macular traction results in morphological tissue alterations and the consequent decline of visual functions.
- Based on the diameter of vitreous attachment to the macular surface measured by an OCT, the International Vitreomacular Traction Study Group subclassifies VMT into:
- focal VMT 1500 µm or less
- broad VMT 1500 µm or more
- Classical symptoms are similar to all vitreomacular diseases: metamorphopsia and decreased visual acuity.
- In daily clinical practice, these changes are only found with OCT. Many cases with VMT are self-limiting but need observation.
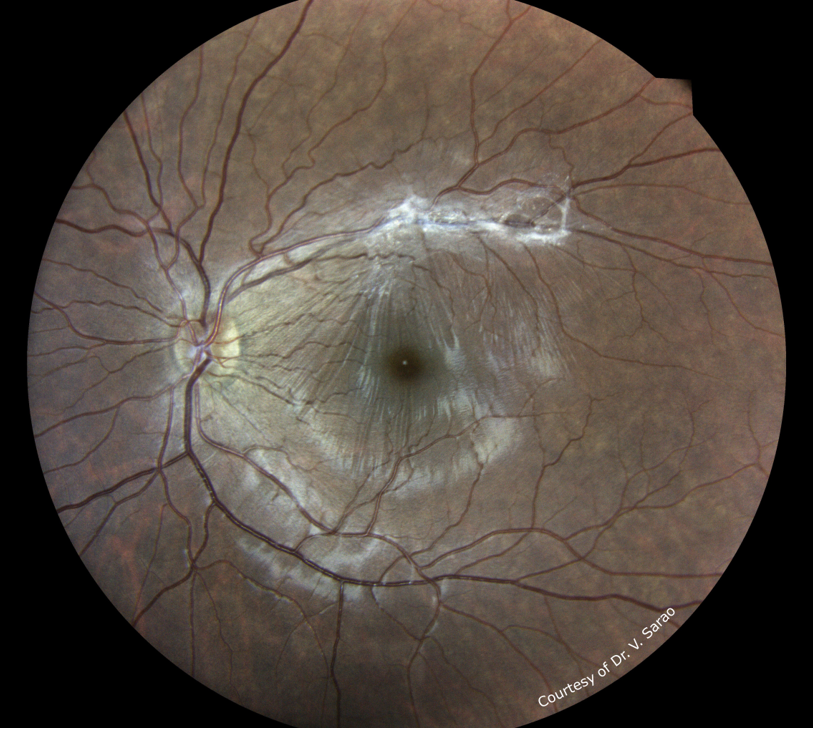

Image 3: Vitreomacular traction
This image was originally published in the Retina Image Bank. Michael P. Kelly, FOPS. Retina Image Bank. Year 2013; Image Number 5141. © the American Society of Retina Specialists.
Image 4: Intraoperative image of a patient with a macular traction syndrome
This image was originally published in the Retina Image Bank. Virgilio Morales-Canton, MD. Retina Image Bank. Year 2012; Image Number 938. © the American Society of Retina Specialists.03
Macular hole
Referral: Urgent if recent onset, if not normal*
A macular hole (MH) is a retinal tissue break involving the fovea (see image 5).
- It is usually idiopathic, but may also be associated with myopia, epiretinal membrane, macular traction, and trauma.
- It can be caused by tangential traction and anterior-posterior traction of the posterior hyaloids on the parafovea.
- Up to 30% of patients have a bilateral hole.
- Patients will usually complain of central scotoma and metamorphosis.
- According to Gass, MH can be divided into four stages. Stage 4 is very clearly visible in fundus images, while stages 1 and 2 are diagnosed with OCT.
-
- Stage 1a: foveal detachment (“yellow dot stage”)
- Stage 1b: yellow ring
- Stage 2: full-thickness macula hole (< 400 µm)
- Stage 3: full-thickness macula hole (> 400 µm) with partial vitreomacular traction
- Stage 4: full-thickness macula hole (> 400 µm) with posterior vitreous detachment


*Referral advice
The referral advice in the atlas should be used as a general guideline. The Optometry Atlas does not establish a standard of optometric care and specific outcomes are not guaranteed. Please read the full details here.



