- This pathology is characterised by increased cupping of the optic disc, with corresponding visual field defect, due to retinal ganglion cell loss.
- Glaucoma is associated with high IOP.
- It tends to run in families. In some people, scientists have identified genes related to high eye pressure and optic nerve damage.
- Types of glaucoma include:
- open-angle glaucoma is the most common form of the disease. The drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked. This causes pressure in the eye to gradually increase. This pressure damages the optic nerve.
- angle-closure glaucoma occurs when the iris bulges forward to narrow or block the drainage angle formed by the cornea and iris. As a result, fluid can’t circulate through the eye and pressure increases. Some people have narrow drainage angles, putting them at increased risk of glaucoma. Acute angle-closure glaucoma is a medical emergency.
- normal-tension glaucoma: the optic nerve becomes damaged even though the eye pressure is within the normal range. No one knows the exact reason for this. The optic nerve may be more sensitive or less blood is supplied to the optic nerve. This limited blood flow could be caused by atherosclerosis or other conditions that impair circulation. (See image 2)
- pigmentary glaucoma: pigment granules from the iris build up in the drainage channels, slowing or blocking fluid exiting the eye. Physical activities sometimes stir up the pigment granules, depositing them on the trabecular meshwork and causing intermittent pressure elevations.
- Pseudoexfoliation glaucoma (PEX): Deposit of material on the corneal endothelium, lens and trabecular meshwork. It is particularly common in Scandinavia.

Chapter 7: Optic nerve conditions
Introduction
This chapter covers the following common optic nerve conditions:
- Glaucoma
- Optic disc drusen
- Optic neuritis
- Papilledema
- Optic atrophy
Click on one of the cards below to read more about the specific eye condition.
Glaucoma
Glaucoma is the most common optic neuropathy in the adulthood. It is defined as a multifactorial optic neuropathy, which is related to abnormal ocular hydrodynamics that damage the optic nerve.



Optic disc drusen
Disc drusen are composed of small proteinaceous material that becomes calcified with advancing age. These deposits can be considered as small tumours that develop within the optic nerve head and may lead to an elevated disc. Therefore, it is sometimes mistaken for papillary oedema.
- Pathogenesis is thought to be related to possibly inherited dysplasia of the optic disc with blood supply comprise, causing slowed axoplasmic flow and leading to the formation of calcific secretion.
- Patients are usually asymptomatic. Rarely, they can have transient visual disturbances (9% of patients).
- Visual field loss is often observed gradually with increasing age, and it has been estimated that a quarter of patients with optic disc drusen have a visual field defect other than an enlarged blind spot.
- If the optic disc drusen are superficial, this can aid in diagnosis during the dilated fundus exam.
The optic nerve usually has a “lumpy-bumpy” appearance:
- elevated, often small, optic disc with indistinct and irregular disc margins.
- drusen seen as round, white/yellow refractile bodies on the surface of the nerve or buried beneath it.
- anomalous vascular branching pattern (tortuosity, opto-ciliary shunt vessels).
- nasal margin is the most common site for drusen.
- over 70 % of the cases are bilateral but asymmetric.


Optic neuritis
Optic neuritis is an inflammation that damages the optic nerve. It's also known as optic nerve papillitis.
- Inflammation usually settle down spontaneously over the weeks. If spontaneous remission does not occur, inflammation is treated with corticosteroids (prednisone or methylprednisolone).
- There are several reasons for optic neuritis. Inflammation, infection (e.g. Syphilis), compressive disorders (tumours) must all be considered. Optic neuritis is also linked to multiple sclerosis (MS), a neuro-degenerative disease of the central nervous system that results from the immune mediated inflammation and demyelination of axons. Signs and symptoms of optic neuritis can be the first indication of MS, or they can occur later in the course of the disease.
- Optic neuritis usually affects one eye. Symptoms may include:
- Pain that is worsened by eye movements. Sometimes the pain feels like a dull ache behind the eyes.
- Vision loss in one eye usually develops over hours or days and improves over several weeks to months. Vision loss is permanent in some cases.
- Visual field loss can occur in any pattern.
- Loss of colour vision often affects colour perception. Colours appear less vivid than normal (especially the bright red colour).
- Flashing lights: some patients may report seeing flashing or flickering lights with eye movements.


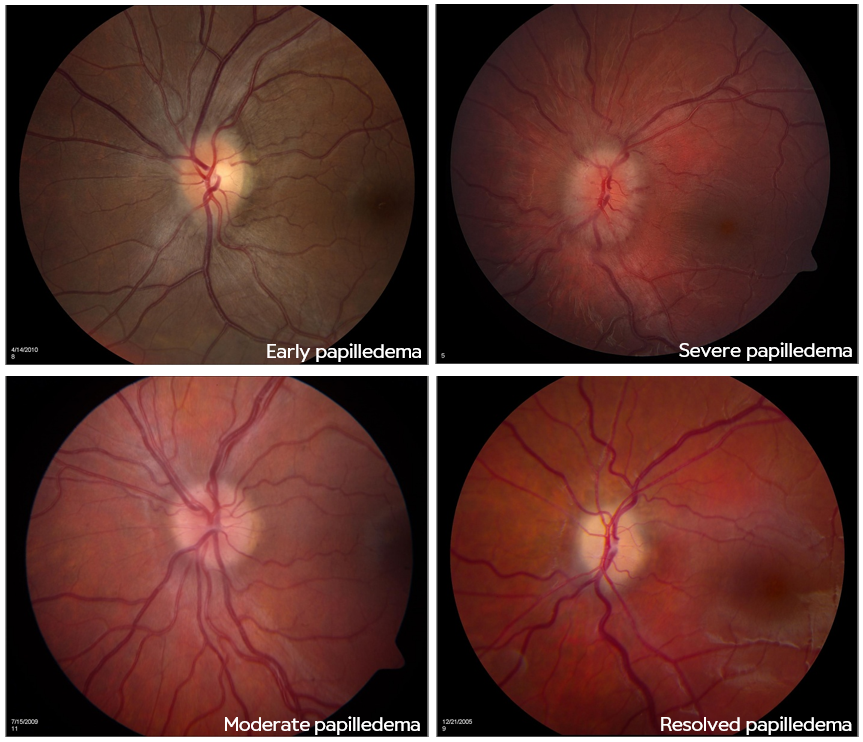
Papilledema
Papilledema refers to bilateral swelling of the optic disc from increased intracranial pressure.
- Papilledema must be distinguished from optic disc swelling from other causes, which is simply termed “optic disc oedema”. Papilledema must also be distinguished from pseudo papilledema such as optic disc drusen.
- The root cause of papilledema is increased intracranial pressure (ICP), which is an alarming sign, and which may presage such entities as a brain tumour, central nervous system inflammation or idiopathic intracranial hypertension.
- Papilledema results from orthograde axoplasmic flow stasis at the optic nerve head leading to oedema of the nerve from the increased intracranial pressure pressing on the nerve behind the eye.
- Continued pressure can result in loss of axons and eventual optic atrophy.
- With optic atrophy, there is little or no oedema seen even with continuing increased intracranial pressure, since there are no fibres left to swell.
Papilledema Grading System (Frisen scale):
- Very early papilledema: obscuration of the nasal border of the disc. No elevation of the disc borders. Normal temporal disc margin.
- Early papilledema: obscuration of all borders. Elevation of the nasal border. Complete peripapillary halo.
- Moderate papilledema: obscurations of all borders. Increased diameter of optic nerve head. Obscuration of one or more segments of major blood vessels. Peripapillary halo – irregular outer fringe with finger-like extensions.
- Marked papilledema: elevation of the entire nerve head. Obscuration of all borders. Peripapillary halo. Total obscuration on the disc of a segment of a major blood vessel.
- Severe papilledema: dome-shaped protrusions representing anterior expansion of the optic nerve head. Peripapillary halo is narrow and smoothly demarcated.
Optic atrophy
Optic atrophy refers to the death of the retinal ganglion cell axons that comprise the optic nerve. Anything that can compromise ganglion cell function can cause optic atrophy over time, and more broadly optic neuropathy.
- The typical sign of optic atrophy is the optic nerve pallor. (See image 9)
- This is the end stage of a process resulting in optic nerve damage anywhere along the path from the retina to the lateral geniculate nucleus.
- Because the optic nerve fibre layer is thinned or absent, the disc margins appear sharp and the disc looks pale, probably reflecting the absence of small vessels in the disc head.
- The main symptom of optic atrophy is vision loss. Any other symptoms are attributable to the underlying process that caused the disc damage (such as pain with angle-closure glaucoma).
- Optic atrophy is usually not difficult to diagnose, because of the characteristic pale optic disc, but the cause for the optic atrophy may be difficult to ascertain. Sometimes the cause of vision loss may be difficult to differentiate between subtle optic neuropathy and disease of the retina (or both).
- Visual field defect patterns include: papillomacular defect (cecocentral scotoma), arcuate defect (include altitudinal) or temporal wedge defect (nasal fibres) for prechiasmal, bitemporal (superior) field defects for chiasmal lesions and hemianopsia for post-chiasmal lesions. (See image 11)



*Referral advice
The referral advice in the atlas should be used as a general guideline. The Optometry Atlas does not establish a standard of optometric care and specific outcomes are not guaranteed. Please read the full details here.



